Combating the Silent Killer: How Pharmaceutical Pollution Fuels the Global Antibiotic Resistance Crisis
“By 2050, antibiotic-resistant illnesses could cause 10 million deaths and $100 trillion in GDP losses globally.”
In today’s interconnected world, we face a looming threat that silently creeps through our communities, endangering human health, agricultural sustainability, and environmental integrity. This threat is the global antibiotic resistance crisis, fueled by pharmaceutical pollution. As we delve into this critical issue, we’ll explore how the mismanagement of pharmaceutical waste is contributing to the rise of “superbugs” and what innovative solutions are being developed to combat this growing menace.
Understanding the Antibiotic Resistance Crisis
Antibiotic resistance occurs when bacteria evolve to withstand the effects of antibiotics, rendering these life-saving drugs ineffective. This phenomenon has been accelerated by the overuse and misuse of antibiotics in healthcare and agriculture. However, a less-discussed but equally alarming contributor to this crisis is pharmaceutical pollution.
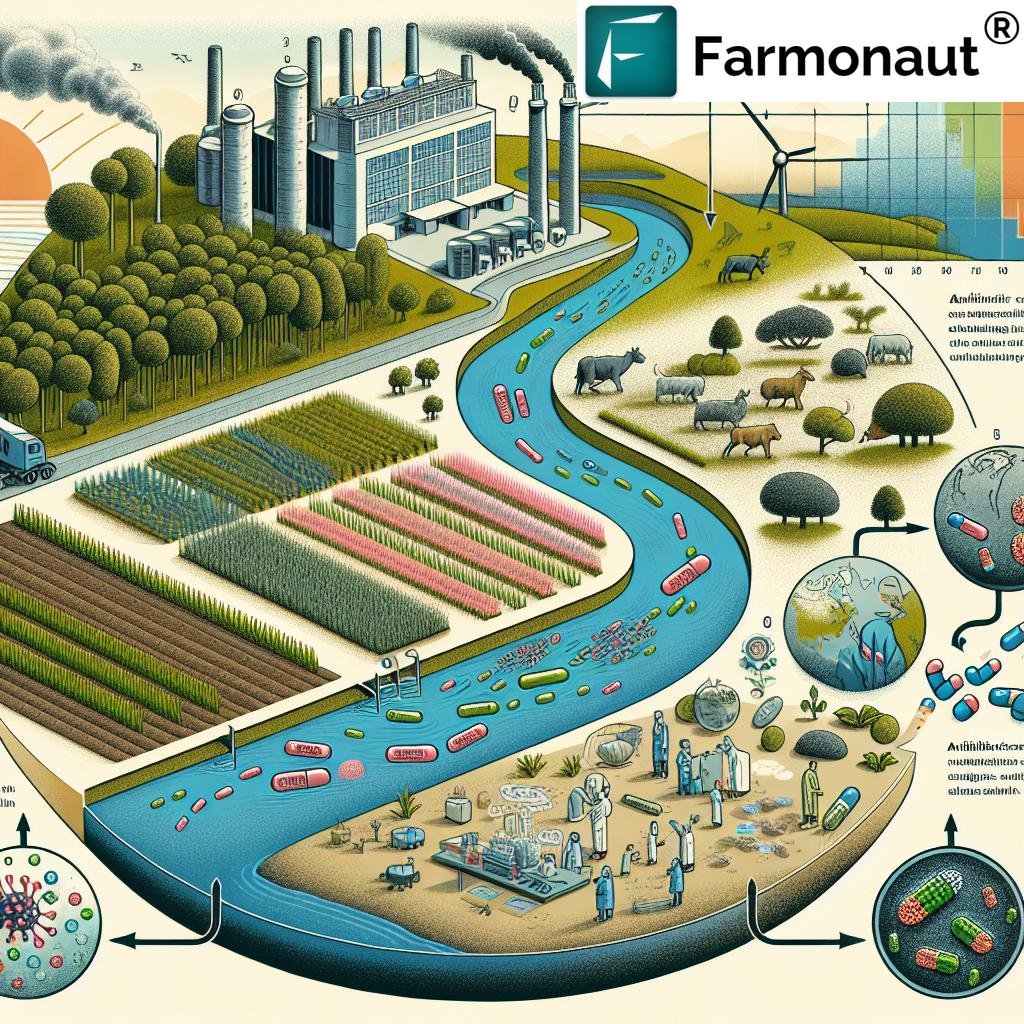
Pharmaceutical pollution refers to the contamination of the environment with pharmaceutical compounds, particularly antibiotics. This pollution primarily stems from poor waste management practices in drug manufacturing facilities. As a result, high concentrations of antibiotics are finding their way into our water supplies, soil, and even the air we breathe.

The Global Scope of the Problem
Research conducted across various regions has revealed alarming levels of pharmaceutical pollution and its impact on antibiotic resistance:
- United States: Studies in the Midwest and Northeast regions have identified elevated concentrations of antibiotics such as azithromycin, ciprofloxacin, sulfamethoxazole, and trimethoprim in water sources.
- Europe: A comprehensive study of the Danube River revealed seven different antibiotic-resistant bacteria strains across a 2,311 km stretch.
- Italy: Researchers discovered 258 active pharmaceutical ingredients in rivers, with an estimated 7-14 tons discharged annually.
- China: Factory studies identified 1,043 viral operational taxonomic units, with 27 resistant genes, 9 of which correlated with 16 highly infectious clinical illnesses.
These findings underscore the global nature of the antibiotic resistance crisis and its intricate connection to pharmaceutical pollution.
The Mechanism of Resistance Development
Bacteria are remarkably adaptable organisms. When exposed to antibiotics in the environment, they can develop resistance through several mechanisms:
- Genetic mutations: Bacteria can undergo spontaneous genetic changes that allow them to analyze and render antibiotics ineffective.
- Horizontal Gene Transfer (HGT): Resistant bacteria can pass their resistance genes to other bacteria, even across species.
- Biofilm formation: Bacteria can create protective layers that reduce antibiotic penetration, allowing them to survive and potentially develop resistance.
The presence of antibiotics in the environment due to pharmaceutical pollution creates an ideal breeding ground for these resistance mechanisms to flourish.
The Spread of Antibiotic-Resistant Bacteria
“High concentrations of antibiotics found in rivers, aquifers, and reservoirs near pharmaceutical factories contribute to ‘superbug’ development.”
The spread of antibiotic-resistant bacteria is not confined to water bodies near pharmaceutical factories. Research has documented the presence of antibiotic-resistant genes (ARGs) in various environments:
- Wildlife: Studies have found 48 multi-drug-resistant genes in 24 parrots and 8-10 ARG compounds in Chilean fish.
- Office spaces: Air samples in office environments have shown higher Colony Forming Units of ARGs.
- Beaches: Microplastics in sand have been found to harbor distinct bacterial communities, potentially including resistant strains.
- Agricultural soil: Contaminated water used for irrigation can introduce resistant bacteria into the soil where our food is grown.
- Air: ARGs have been detected in air samples from common public spaces.
This widespread distribution of antibiotic-resistant bacteria poses a significant threat to human health, animal welfare, and environmental integrity.
The Economic and Health Impact
The antibiotic resistance crisis is not just a health concern; it’s also an economic one. Projections estimate that by 2050, antibiotic-resistant illnesses could cause:
- 10 million deaths worldwide annually
- Up to $100 trillion in GDP losses globally
These staggering figures underscore the urgent need for action to address this growing crisis.
The Role of Regulation and Oversight
One of the most concerning aspects of the pharmaceutical pollution problem is the lack of robust regulatory oversight. Currently, only eight major pharmaceutical factories worldwide have set regulations on the permissible levels of antibiotics in their wastewater. This regulatory gap allows for the continued release of high concentrations of antibiotics into the environment.
Moreover, many manufacturing plants are located in areas with lax environmental regulations, often in lower socioeconomic regions. This situation creates a perfect storm for the proliferation of antibiotic-resistant bacteria.
Innovative Solutions to Combat the Crisis
Addressing the antibiotic resistance crisis requires a multi-faceted approach. Here are some innovative solutions being developed and implemented:
- Advanced Filtration Systems: Researchers are developing sophisticated filtration systems using combinations of gravel, sand, soil, and biochar to remove antibiotics from wastewater effectively.
- Water Reuse in Pharmaceutical Manufacturing: Implementing closed-loop systems in pharmaceutical factories can significantly reduce the release of antibiotics into the environment.
- Global Standards for Contaminant Levels: Establishing and enforcing international standards for acceptable levels of pharmaceutical contaminants in wastewater is crucial.
- Increased Transparency and Accountability: Encouraging greater transparency between pharmaceutical companies and governing bodies can lead to more effective regulation and compliance.
- Government Regulations: Implementing strict governmental regulations on pharmaceutical waste management, especially in areas with high concentrations of manufacturing facilities.
The One Health Approach
To effectively combat the antibiotic resistance crisis, we need to adopt a “One Health” approach. This holistic strategy recognizes that the health of humans, animals, and the environment are interconnected. By addressing the issue from multiple angles simultaneously, we can create more effective and sustainable solutions.
The One Health approach involves:
- Collaboration between healthcare professionals, veterinarians, and environmental scientists
- Integrated surveillance of antibiotic resistance in humans, animals, and the environment
- Development of alternative therapies to reduce reliance on antibiotics
- Education and awareness programs to promote responsible antibiotic use
The Role of Technology in Monitoring and Prevention
Advanced technologies are playing a crucial role in monitoring and preventing the spread of antibiotic-resistant bacteria. For instance, Farmonaut, a leading agricultural technology company, offers innovative solutions that can indirectly contribute to combating this crisis:
- Satellite-Based Crop Health Monitoring: By providing real-time data on crop health, Farmonaut’s technology can help reduce the overuse of antibiotics in agriculture. Farmers can make more informed decisions about pest management and resource allocation, potentially decreasing the need for antibiotic use in livestock.
- AI-Driven Advisory Systems: Farmonaut’s Jeevn AI system offers personalized farm management advice, which can include strategies for sustainable pest control and crop health maintenance without relying heavily on antibiotics.
- Blockchain-Based Traceability: This technology can help track the use of antibiotics in the food supply chain, promoting transparency and accountability.
While Farmonaut’s primary focus is on agricultural technology, its solutions demonstrate how innovative approaches in related fields can contribute to addressing the broader issue of antibiotic resistance.
Public Awareness and Education
One of the most powerful tools in combating the antibiotic resistance crisis is public awareness. By educating communities about the dangers of antibiotic misuse and the importance of proper pharmaceutical waste management, we can drive change from the ground up.
Key areas for public education include:
- Proper disposal of unused medications
- Understanding when antibiotics are necessary and when they’re not
- The importance of completing full courses of prescribed antibiotics
- Recognizing the environmental impact of pharmaceutical pollution
The Way Forward
Addressing the global antibiotic resistance crisis fueled by pharmaceutical pollution requires a concerted effort from governments, industries, researchers, and the public. By implementing stricter regulations, developing innovative technologies, and raising awareness, we can work towards mitigating this silent killer.
As we move forward, it’s crucial to remember that this is not just a health issue or an environmental issue – it’s a global challenge that affects every aspect of our lives. By taking action now, we can protect our communities, preserve the effectiveness of life-saving antibiotics, and ensure a healthier future for generations to come.
Explore Farmonaut’s API for advanced agricultural insights
Access Farmonaut’s API Developer Docs
Comparative Analysis of Antibiotic Resistance Impact
| Sector | Current Impact | Projected Impact by 2050 | Economic Cost (Billions USD) | Potential Solutions |
|---|---|---|---|---|
| Healthcare | 700,000 deaths annually | 10 million deaths annually | 100,000 | New antibiotic development, improved diagnostics, antibiotic stewardship programs |
| Agriculture | Decreased livestock productivity | Significant food security threats | 20,000 | Reduced antibiotic use in animals, improved farming practices, alternative growth promoters |
| Environment | Widespread contamination of water bodies | Ecosystem collapse in heavily polluted areas | 5,000 | Advanced wastewater treatment, stricter regulations on pharmaceutical waste, environmental monitoring |
| Economy | 0.5% reduction in GDP globally | 3.8% reduction in GDP globally | 100,000 | Investment in R&D, international cooperation, economic incentives for antibiotic development |
FAQ Section
Q: What is antibiotic resistance?
A: Antibiotic resistance occurs when bacteria evolve to survive the effects of antibiotics, making these drugs ineffective in treating infections.
Q: How does pharmaceutical pollution contribute to antibiotic resistance?
A: Pharmaceutical pollution releases high concentrations of antibiotics into the environment, creating conditions where bacteria are exposed to these drugs and can develop resistance mechanisms.
Q: What are “superbugs”?
A: “Superbugs” are bacteria that have developed resistance to multiple types of antibiotics, making them extremely difficult to treat and potentially life-threatening.
Q: How can individuals help combat antibiotic resistance?
A: Individuals can help by using antibiotics only when prescribed, completing the full course of antibiotics, and properly disposing of unused medications.
Q: What is the “One Health” approach to antibiotic resistance?
A: The “One Health” approach recognizes the interconnectedness of human, animal, and environmental health, addressing antibiotic resistance through collaborative efforts across these sectors.
Earn With Farmonaut: Affiliate Program
Earn 20% recurring commission with Farmonaut’s affiliate program by sharing your promo code and helping farmers save 10%. Onboard 10 Elite farmers monthly to earn a minimum of $148,000 annually—start now and grow your income!
Farmonaut Subscriptions
In conclusion, the global antibiotic resistance crisis, fueled by pharmaceutical pollution, is a complex challenge that requires immediate and coordinated action. By implementing innovative solutions, leveraging technology, and raising public awareness, we can work towards mitigating this silent killer and preserving the effectiveness of antibiotics for future generations.