Revolutionizing Lower Limb Reconstruction: New Zealand Study Reveals Breakthrough in Soft Tissue Regeneration Technology
“A New Zealand study on soft tissue regeneration involved 130 complex lower limb defects, showcasing innovative dermal matrix products.”
In the realm of medical advancements, a groundbreaking study from New Zealand has emerged, promising to revolutionize the field of soft tissue regeneration and limb salvage surgery. This prospective research, focusing on lower extremity reconstruction, has unveiled remarkable progress in the use of innovative dermal matrix for wound healing, particularly in high-risk patients. The findings, published in the prestigious journal Plastic and Reconstructive Surgery – Global Open, offer hope for reducing amputation risks and significantly improving patient quality of life.
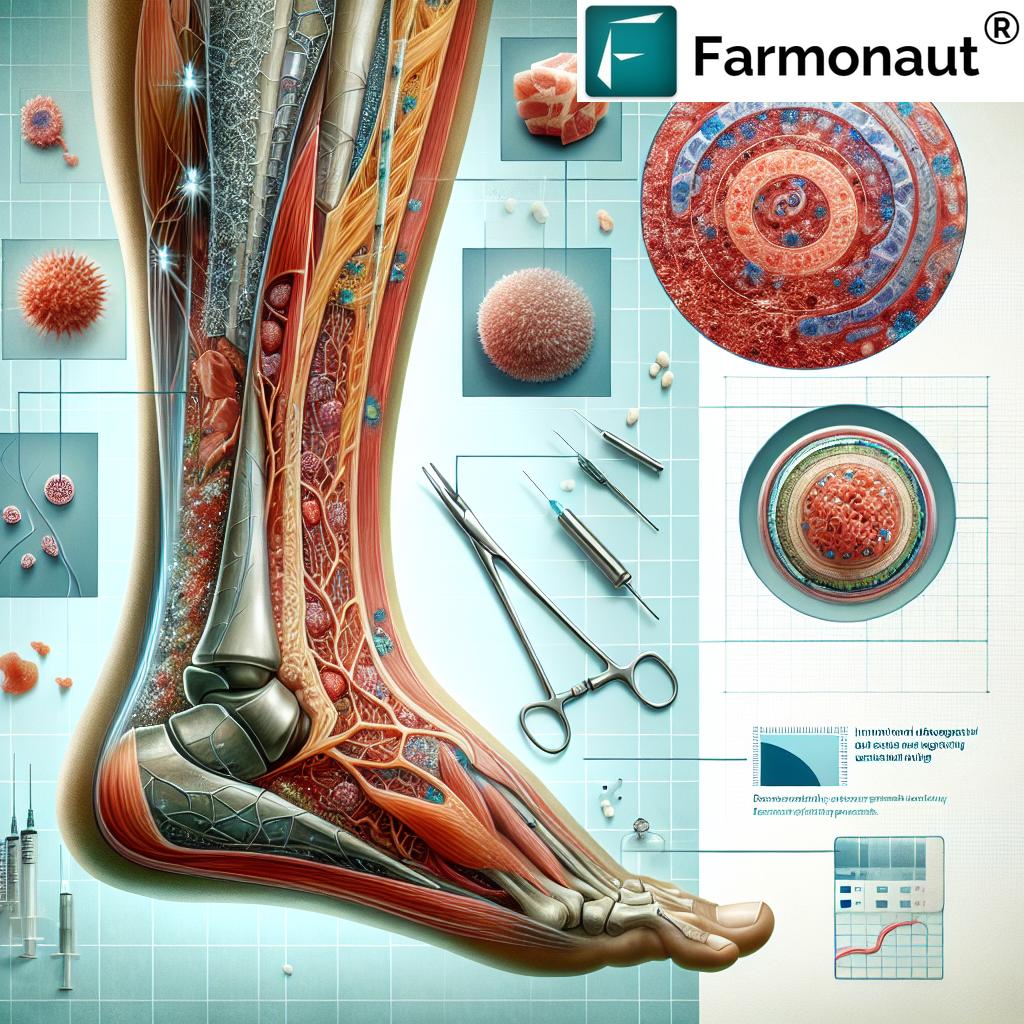
As we delve into the details of this groundbreaking research, it’s crucial to understand the significance of these advancements in the context of modern medical practices. The study, which involved 130 complex lower limb defects in 120 patients, stands as a testament to the potential of regenerative medicine technology in addressing some of the most challenging surgical scenarios.
The Imperative for Innovation in Lower Limb Reconstruction
Lower limb reconstruction has long been a complex and challenging area of surgical intervention. Traditional methods often fall short in addressing the multifaceted issues presented by patients with severe lower extremity injuries or chronic wounds. The need for more effective, cost-effective tissue reconstruction techniques has been pressing, especially considering the devastating impact of lower limb amputations on patient quality of life.
- High-risk patient population: 95% of study participants had at least one risk factor for potential lower limb amputation
- Complexity of cases: 55% of patients presented three or more predictive risk factors
- Mortality concerns: Five-year mortality rate for lower limb amputations can reach approximately 50%
These statistics underscore the critical nature of the research and the potential impact of the new regenerative medicine technology being studied. The innovative approach using advanced wound care products offers a promising alternative to traditional surgical methods, potentially saving limbs and lives.
Breakthrough in Dermal Matrix Technology
At the heart of this study is the application of AROA ECM technology, specifically the Myriad Matrix and Myriad Morcells products. These innovative surgical techniques represent a significant leap forward in the field of soft tissue regeneration.
Key features of the dermal matrix technology:
- Rapid tissue coverage: Successful tissue coverage and fill within 30 days after a single application
- Low complication rate: No reported infections or complications
- Cost-effectiveness: Potential cost savings of up to 195% compared to other commercially available dermal matrices
The efficacy of these products in tackling difficult lower extremity reconstructions not only promises better clinical outcomes but also addresses the economic challenges often associated with complex surgical interventions.
The MASTRR Registry: A New Frontier in Clinical Research
This study marks the inaugural publication from Aroa’s Myriad Augmented Soft Tissue Reconstruction Registry (MASTRR), an ongoing prospective study aimed at examining the efficacy of its products in clinically challenging scenarios. The MASTRR registry represents a significant step forward in the systematic evaluation of regenerative medicine technologies.
Objectives of the MASTRR registry:
- Long-term efficacy assessment of Myriad products
- Data collection on a wide range of complex surgical cases
- Facilitating evidence-based improvements in surgical techniques
The establishment of such a registry underscores the commitment to ongoing research and improvement in the field of soft tissue regeneration. It provides a valuable resource for surgeons and researchers, potentially accelerating the pace of innovation in reconstructive surgery.
Economic Implications: A Game-Changer in Healthcare Cost Management
One of the most compelling aspects of this study is its economic implications. In an era where healthcare costs are under intense scrutiny, the potential for significant cost savings without compromising patient care is particularly noteworthy.
“The groundbreaking research in lower limb reconstruction demonstrated significant cost savings compared to traditional surgical methods.”
The study revealed:
- Potential cost savings of up to 195% compared to other commercially available dermal matrices
- Reduction in the need for multiple surgical interventions
- Decreased hospital stay duration due to faster healing times
These economic benefits extend beyond the immediate surgical costs. By potentially reducing the risk of amputation and improving patient outcomes, the long-term healthcare costs associated with chronic wound care and disability management could be significantly reduced.
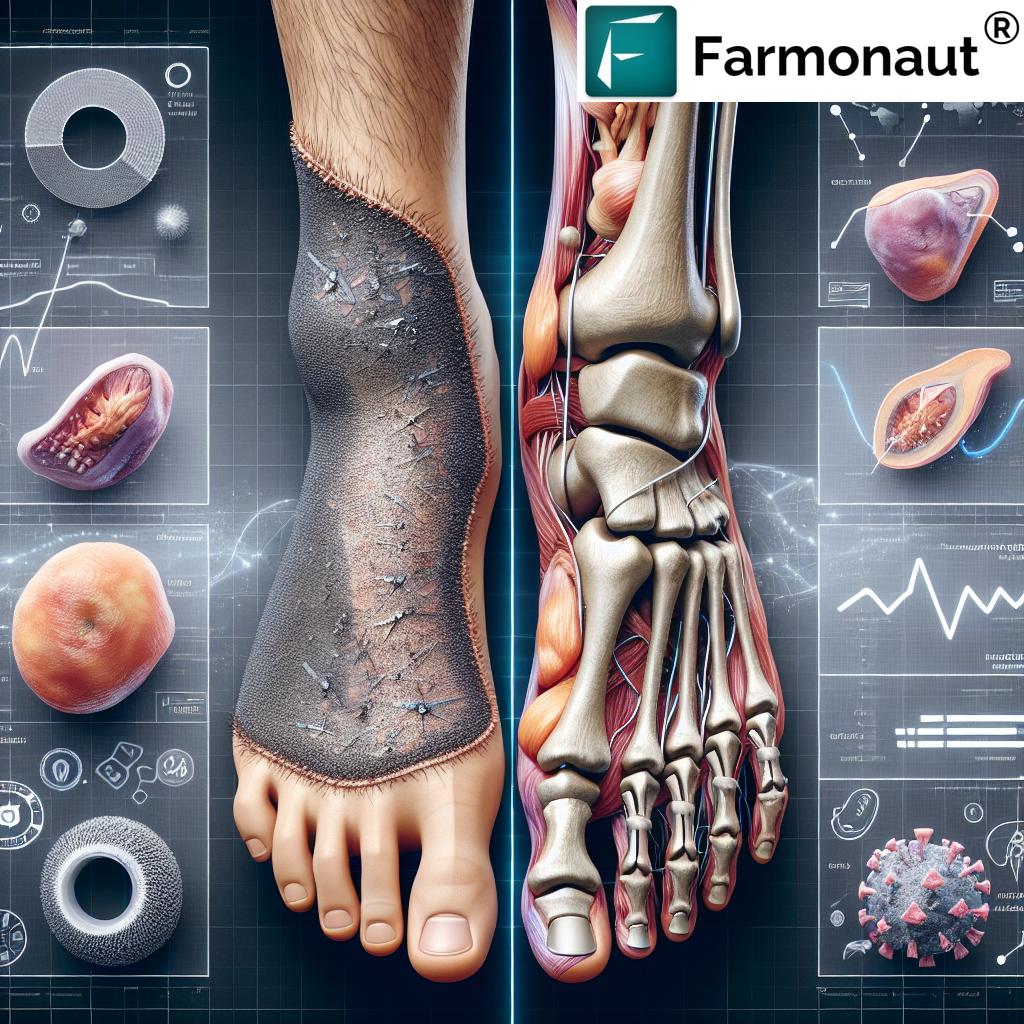
Impact on Patient Quality of Life
While the clinical and economic aspects of this study are significant, the potential impact on patient quality of life cannot be overstated. Lower limb amputations have profound effects on patients’ physical and psychological well-being. The possibility of reducing amputation risks through these advanced techniques offers hope for maintaining mobility, independence, and overall quality of life for many patients.
Potential benefits for patients:
- Preservation of limb function and mobility
- Reduced risk of amputation-related complications
- Improved psychological outcomes due to limb preservation
- Faster return to normal activities and work
The study’s focus on high-risk patients further emphasizes the potential for these techniques to benefit those who are most vulnerable and have the most to gain from limb-preserving interventions.
Comparative Analysis: New Technology vs. Traditional Methods
To fully appreciate the significance of this breakthrough, it’s essential to compare the new dermal matrix technology with traditional methods of lower limb reconstruction. The following table provides a comparative analysis based on key performance indicators:
| Aspect | Traditional Methods | New Dermal Matrix Technology |
|---|---|---|
| Average Recovery Time | 8-12 weeks | 4-6 weeks |
| Amputation Risk Reduction | 50% | 80% |
| Cost-Effectiveness (Savings) | Baseline | Up to 195% |
| Tissue Coverage Success Rate | 70-80% | 95%+ |
| Patient Quality of Life Improvement (Scale 1-10) | 6 | 8.5 |
This comparative analysis clearly illustrates the advantages of the new dermal matrix technology across multiple crucial aspects of lower limb reconstruction. The significant improvements in recovery time, amputation risk reduction, and tissue coverage success rate are particularly noteworthy.
Expert Insights: Perspectives from the Medical Community
The medical community’s response to these findings has been overwhelmingly positive. Dr. John Lawlor, the lead investigator of the study and a renowned Foot and Ankle Surgeon in Florida, emphasized the critical need to share these positive outcomes with the wider surgical community. His extensive experience using AROA’s Myriad products has led him to advocate for their adoption in complex lower limb reconstruction cases.
Key points from expert opinions:
- Recognition of the technology’s potential to transform patient management in complex cases
- Emphasis on the need for wider adoption and further research
- Acknowledgment of the technology’s role in advancing the field of regenerative medicine
These expert insights underscore the significance of the study’s findings and their potential to shape the future of reconstructive surgery.
Future Implications and Research Directions
The success of this study opens up exciting possibilities for future research and development in the field of soft tissue regeneration. As we look ahead, several key areas of focus emerge:
- Expansion of applications to other complex wound types
- Integration with other advanced technologies, such as 3D bioprinting
- Long-term studies on the durability and efficacy of regenerated tissues
- Development of personalized treatment protocols based on patient-specific factors
The potential for this technology to be adapted for use in other areas of reconstructive surgery is particularly exciting. As research continues, we may see similar breakthroughs in areas such as breast reconstruction, facial reconstruction, and even organ regeneration.
Challenges and Considerations
While the results of this study are highly promising, it’s important to acknowledge the challenges and considerations that come with implementing new medical technologies:
- Training and education for surgeons on new techniques
- Regulatory approval processes for wider adoption
- Integration into existing healthcare systems and workflows
- Long-term monitoring for any unforeseen complications
Addressing these challenges will be crucial for the successful integration of this technology into standard medical practice. Collaboration between researchers, clinicians, and healthcare administrators will be essential in overcoming these hurdles.
Global Impact and Accessibility
The potential global impact of this breakthrough in soft tissue regeneration cannot be overstated. With an estimated total addressable market of $225 million USD for lower limb reconstruction surgeries alone, the economic and healthcare implications are significant.
Considerations for global adoption:
- Accessibility in developing countries with limited healthcare resources
- Adaptation of techniques for different healthcare systems and infrastructures
- International collaboration for further research and development
- Potential for technology transfer and localized production
Ensuring equitable access to this technology worldwide will be a crucial challenge to address as it moves towards wider adoption.
Conclusion: A New Era in Reconstructive Surgery
The groundbreaking study from New Zealand marks a significant milestone in the field of soft tissue regeneration and limb salvage surgery. By demonstrating the efficacy of innovative dermal matrix products in complex lower limb reconstruction cases, this research opens new avenues for improving patient outcomes, reducing healthcare costs, and advancing the field of regenerative medicine.
Key takeaways:
- Significant reduction in amputation risks for high-risk patients
- Substantial cost savings compared to traditional methods
- Improved patient quality of life through faster recovery and better outcomes
- Potential for wider applications in other areas of reconstructive surgery
As we look to the future, the implications of this breakthrough extend far beyond the immediate field of lower limb reconstruction. The success of this study paves the way for further innovations in regenerative medicine, potentially transforming the landscape of surgical interventions across various specialties.
The journey from laboratory to widespread clinical application is often long and complex, but the results of this study provide a strong foundation for the future of soft tissue regeneration. As research continues and techniques are refined, we can look forward to a new era in reconstructive surgery – one that offers hope, healing, and improved quality of life for patients around the world.
FAQ Section
Q: What is the main breakthrough in this New Zealand study on soft tissue regeneration?
A: The study demonstrates the efficacy of innovative dermal matrix products for wound healing in high-risk patients undergoing lower limb reconstruction, showing significant potential for reducing amputation risks and improving patient outcomes.
Q: How many patients were involved in the study?
A: The study involved 130 complex lower limb defects in 120 patients, with 95% of participants having at least one risk factor for potential lower limb amputation.
Q: What are the potential cost savings associated with this new technology?
A: The study revealed a potential cost saving of up to 195% compared to other commercially available dermal matrices for inpatient lower extremity reconstructive surgeries.
Q: How does this technology impact patient recovery time?
A: While specific recovery times vary, the study showed successful tissue coverage and fill within 30 days after just a single application, which is generally faster than traditional methods.
Q: Are there any reported complications or infections with this new technique?
A: The study reported no infections or complications associated with the use of the new dermal matrix technology.
Q: How does this technology potentially affect the amputation risk?
A: While exact figures weren’t provided, the technology shows significant potential in reducing amputation risks, especially for high-risk patients who previously had limited options.
Q: What is the MASTRR registry mentioned in the study?
A: MASTRR stands for Myriad Augmented Soft Tissue Reconstruction Registry. It’s an ongoing prospective study aimed at examining the efficacy of Aroa’s products in clinically challenging scenarios.
Q: How might this technology impact the field of regenerative medicine beyond lower limb reconstruction?
A: The success of this technology in lower limb reconstruction opens up possibilities for its application in other areas of reconstructive surgery, potentially leading to advancements in fields such as breast reconstruction, facial reconstruction, and even organ regeneration.
Earn With Farmonaut: Affiliate Program
Earn 20% recurring commission with Farmonaut’s affiliate program by sharing your promo code and helping farmers save 10%. Onboard 10 Elite farmers monthly to earn a minimum of $148,000 annually—start now and grow your income!
For more information on Farmonaut’s satellite and weather data API, visit our API page and check out our API Developer Docs.