Breaking the Cycle: How Positive Experiences Combat Childhood Trauma and Obesity in Auckland

“87% of children in New Zealand experience at least one traumatic event by age eight, doubling their obesity risk.”
In the vibrant city of Auckland, New Zealand, a pressing health concern has emerged that demands our immediate attention. The intricate link between childhood trauma and obesity has become increasingly apparent, with recent research shedding light on the profound impact of adverse childhood experiences on physical health. As we delve into this critical issue, we’ll explore the complex relationship between early life stress and obesity, and more importantly, discover how positive experiences can break this cycle and pave the way for healthier futures.
Understanding the Link: Childhood Trauma and Obesity
The connection between childhood trauma and obesity is far from simple. It’s a multifaceted issue that intertwines psychological, physiological, and social factors. Let’s break down this relationship to better understand its implications:
- Prevalence of Childhood Trauma: A groundbreaking study utilizing data from the Growing Up in New Zealand initiative revealed that a staggering 87% of nearly 5,000 children faced at least one serious source of trauma by the age of eight.
- Types of Trauma: These adverse childhood experiences include abuse, bullying, exposure to domestic violence, and parental mental health issues, among others.
- Increased Obesity Risk: Children who experienced at least one traumatic event were found to be twice as likely to be obese by age eight, with the risk increasing with the number and severity of the experiences.
- Vulnerable Populations: Alarmingly, children from financially disadvantaged backgrounds and those belonging to Maori and Pasifika communities reported higher rates of trauma.
This data paints a concerning picture of the challenges faced by Auckland’s young population. However, understanding these statistics is the first step towards implementing effective solutions.
The Physiological Impact of Childhood Stress
Childhood stress can have far-reaching effects on a child’s physical health, particularly in relation to obesity. Here’s how early life adversity can lead to increased obesity risk:
- Stress Response: Traumatic experiences trigger the body’s stress response, leading to elevated cortisol levels. Chronic elevation of cortisol can disrupt metabolism and promote fat storage, especially around the abdominal area.
- Emotional Eating: Children may turn to food as a coping mechanism for emotional distress, often favoring high-calorie “comfort” foods.
- Disrupted Sleep Patterns: Trauma can affect sleep quality and duration, which in turn can impact appetite regulation and metabolism.
- Reduced Physical Activity: Traumatized children may be less likely to engage in physical activities, preferring sedentary behaviors as a form of self-protection or due to depression.
Understanding these physiological responses is crucial in developing targeted interventions to break the cycle of trauma and obesity.
The Power of Positive Experiences
“Engaging in enriching activities and maintaining healthy routines can reduce childhood obesity risk by up to 60%.”
While the statistics on childhood trauma and obesity are alarming, there’s a silver lining that offers hope. The same research that highlighted the risks also revealed the transformative power of positive experiences in mitigating these challenges. Let’s explore how positive influences can make a significant difference:
- Protective Effect: Children who were engaged in enriching activities, maintained healthy routines, and attended quality educational programs were significantly less likely to be obese.
- Quantifiable Impact: Children with five or six positive experiences were 60% less likely to be overweight compared to those with no positive experiences.
- Cumulative Benefits: Even two positive experiences led to a 25% reduction in the likelihood of obesity, showcasing that every positive interaction counts.
- Balancing Act: A minimum of four positive experiences is necessary to substantially offset the negative consequences of adverse events.
These findings underscore the importance of creating supportive and enriching environments for children, particularly those who have faced trauma. By fostering positive experiences, we can protect children from the adverse effects of trauma while promoting their overall wellbeing.

Strategies for Promoting Positive Experiences
To effectively combat the impact of childhood trauma on obesity, we need to focus on creating and promoting positive experiences. Here are some strategies that can make a significant difference:
- Structured After-School Programs: Engaging children in organized activities after school can provide routine, social interaction, and physical activity.
- Family Routines: Establishing consistent family routines, such as regular mealtimes and bedtimes, can provide stability and security.
- Quality Education: Ensuring access to high-quality educational programs that foster curiosity and learning can be a powerful positive experience.
- Community Initiatives: Local community programs that offer safe spaces for play, learning, and social interaction can be invaluable.
- Mental Health Support: Providing access to age-appropriate mental health services can help children process trauma and develop coping skills.
By implementing these strategies, we can create a network of support that helps children build resilience and maintain healthy lifestyles.
The Role of Trauma-Informed Care
Addressing childhood obesity in the context of trauma requires a specialized approach. Trauma-informed care is an essential component of this strategy. Here’s why it’s crucial:
- Holistic Approach: Trauma-informed care considers the whole child, recognizing that behaviors and health issues may be rooted in past experiences.
- Safety and Trust: It creates environments where children feel safe and can build trusting relationships with caregivers and healthcare providers.
- Empowerment: This approach empowers children by giving them choices and involving them in decisions about their health and wellbeing.
- Avoiding Re-traumatization: Trauma-informed practices are designed to prevent inadvertently causing additional stress or trauma during treatment.
By incorporating trauma-informed care into obesity prevention and treatment programs, we can address the root causes of the issue more effectively.
The Impact of Positive Experiences on Childhood Obesity Risk
| Positive Experience | Estimated Obesity Risk Reduction (%) |
|---|---|
| Engaging in enriching activities | 40% |
| Maintaining healthy routines | 35% |
| Attending quality educational programs | 30% |
| Participating in community initiatives | 25% |
| Having supportive family relationships | 50% |
| Experiencing five or more positive influences | 60% |
This table clearly illustrates the significant impact that positive experiences can have on reducing childhood obesity risk. It’s evident that a combination of these experiences can substantially decrease the likelihood of obesity, with supportive family relationships and a cumulative effect of multiple positive influences showing the most dramatic reductions.
The Role of Family and Community
Families and communities play a pivotal role in creating positive experiences and mitigating the effects of childhood trauma. Here’s how they can contribute:
- Supportive Home Environment: Parents can create a nurturing home environment that provides emotional support and promotes healthy habits.
- Community Programs: Local initiatives can offer safe spaces for children to play, learn, and interact with peers.
- Cultural Sensitivity: Programs that respect and incorporate cultural traditions can be particularly effective for Maori and Pasifika communities.
- Peer Support Groups: Connecting children who have experienced trauma with supportive peer groups can foster resilience and positive social interactions.
By strengthening these support systems, we can create a more robust network of positive experiences for vulnerable children.
Policy Implications and Recommendations
Addressing the link between childhood trauma and obesity requires a concerted effort at the policy level. Here are some recommendations for policymakers in Auckland and beyond:
- Integrated Health Services: Develop policies that integrate mental health services with obesity prevention programs.
- School-Based Interventions: Implement comprehensive school health programs that address both physical and emotional wellbeing.
- Community Funding: Allocate resources to community-based programs that provide positive experiences for at-risk children.
- Training for Professionals: Ensure that healthcare providers, educators, and social workers receive training in trauma-informed care.
- Research Support: Continue to fund research that explores the relationship between childhood experiences and health outcomes.
By implementing these policies, we can create a more supportive environment for children to thrive both physically and emotionally.
The Future of Childhood Obesity Prevention
As we look to the future, it’s clear that addressing childhood obesity requires a multifaceted approach that goes beyond traditional weight management programs. Here are some innovative strategies that show promise:
- Technology-Assisted Interventions: Utilizing mobile apps and wearable devices to promote healthy behaviors and track progress.
- Personalized Nutrition Plans: Developing individualized nutrition strategies that consider a child’s unique experiences and preferences.
- Virtual Reality Therapy: Using VR to create safe, immersive environments for children to process trauma and learn coping skills.
- Social-Emotional Learning Programs: Integrating SEL into school curricula to help children develop emotional regulation and resilience.
These innovative approaches, combined with traditional methods, can pave the way for more effective obesity prevention strategies.
Conclusion: Breaking the Cycle
The relationship between childhood trauma and obesity is complex, but not insurmountable. By understanding the impact of adverse childhood experiences and harnessing the power of positive influences, we can break the cycle and promote healthier futures for children in Auckland and beyond. It’s crucial that we approach this issue with compassion, recognizing that behind every statistic is a child deserving of support and opportunity.
As we move forward, let’s commit to creating environments where every child has access to the positive experiences they need to thrive. By doing so, we’re not just combating childhood obesity; we’re nurturing resilient, healthy individuals who can reach their full potential.
Together, we can build a future where childhood trauma no longer dictates health outcomes, and where every child has the opportunity to grow, learn, and flourish in a supportive and nurturing environment.
FAQ Section
- Q: How common is childhood trauma in Auckland?
A: According to recent studies, 87% of children in Auckland experience at least one traumatic event by age eight. - Q: What types of trauma are most associated with childhood obesity?
A: Physical abuse, domestic violence, and severe neglect show the strongest associations with childhood obesity. - Q: How much can positive experiences reduce obesity risk?
A: Children with five or six positive experiences were found to have up to a 60% reduced risk of obesity. - Q: What are some examples of positive experiences that can help?
A: Engaging in enriching activities, maintaining healthy routines, attending quality educational programs, and having supportive family relationships are all beneficial. - Q: Are certain communities more at risk?
A: Yes, children from financially disadvantaged backgrounds and those belonging to Maori and Pasifika communities reported higher rates of trauma and subsequent obesity risk. - Q: How can parents help create positive experiences?
A: Parents can establish consistent family routines, engage children in beneficial activities, provide emotional support, and create a nurturing home environment. - Q: What role do schools play in addressing this issue?
A: Schools can implement trauma-informed practices, offer quality educational programs, provide opportunities for physical activity, and support social-emotional learning. - Q: How does trauma-informed care help in obesity prevention?
A: Trauma-informed care addresses the root causes of obesity by considering the whole child, creating safe environments, and avoiding re-traumatization during treatment. - Q: What policy changes could help address this issue?
A: Policies that integrate mental health services with obesity prevention programs, fund community initiatives, and support research into childhood experiences and health outcomes are crucial. - Q: How can communities support children at risk?
A: Communities can offer safe spaces for play and learning, provide culturally sensitive programs, and create peer support networks for children who have experienced trauma.
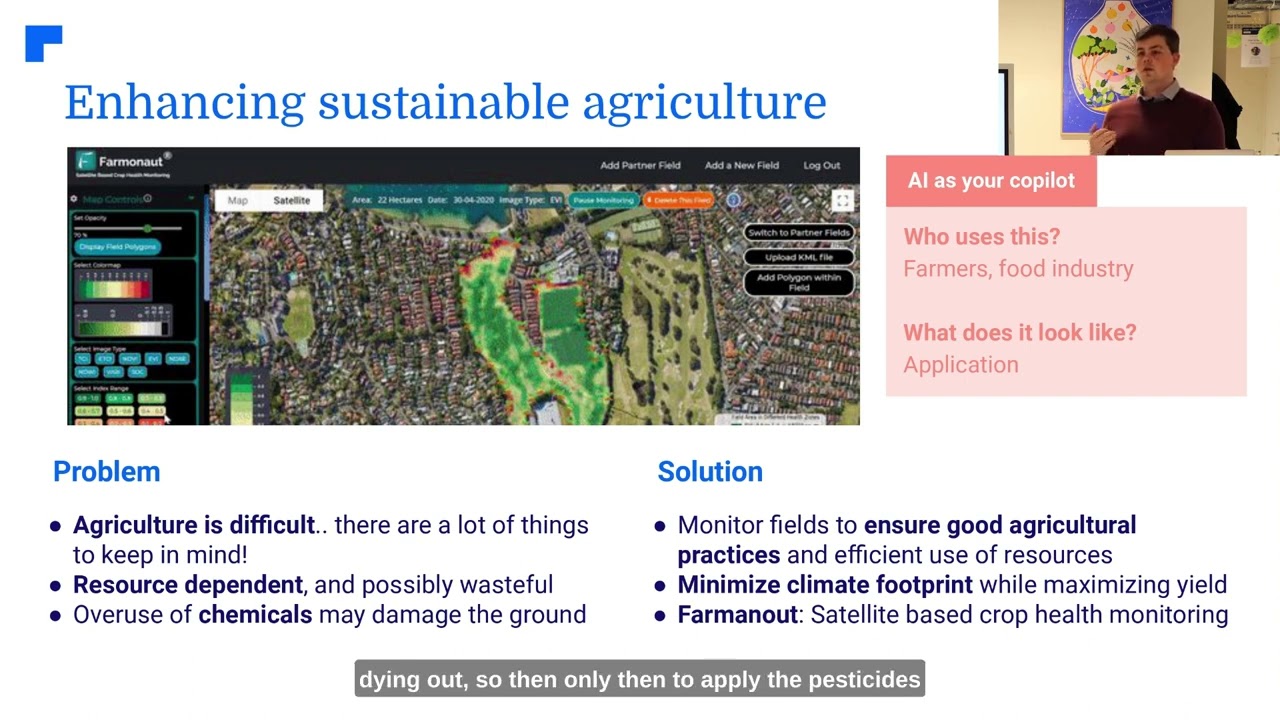
Earn With Farmonaut: Join our affiliate program and earn a 20% recurring commission by sharing your promo code and helping farmers save 10%. Onboard 10 Elite farmers monthly to earn a minimum of $148,000 annually—start now and grow your income!
For more information on our innovative agricultural solutions, visit our API page or check out our API Developer Docs.
Download our apps to stay connected: