COVID-19 Recovery Alert: Understanding Valley Fever Risk and Symptoms in Southwestern US
“Valley Fever, found in arid southwestern US, poses a new threat to 100% of post-COVID patients with compromised immune systems.”
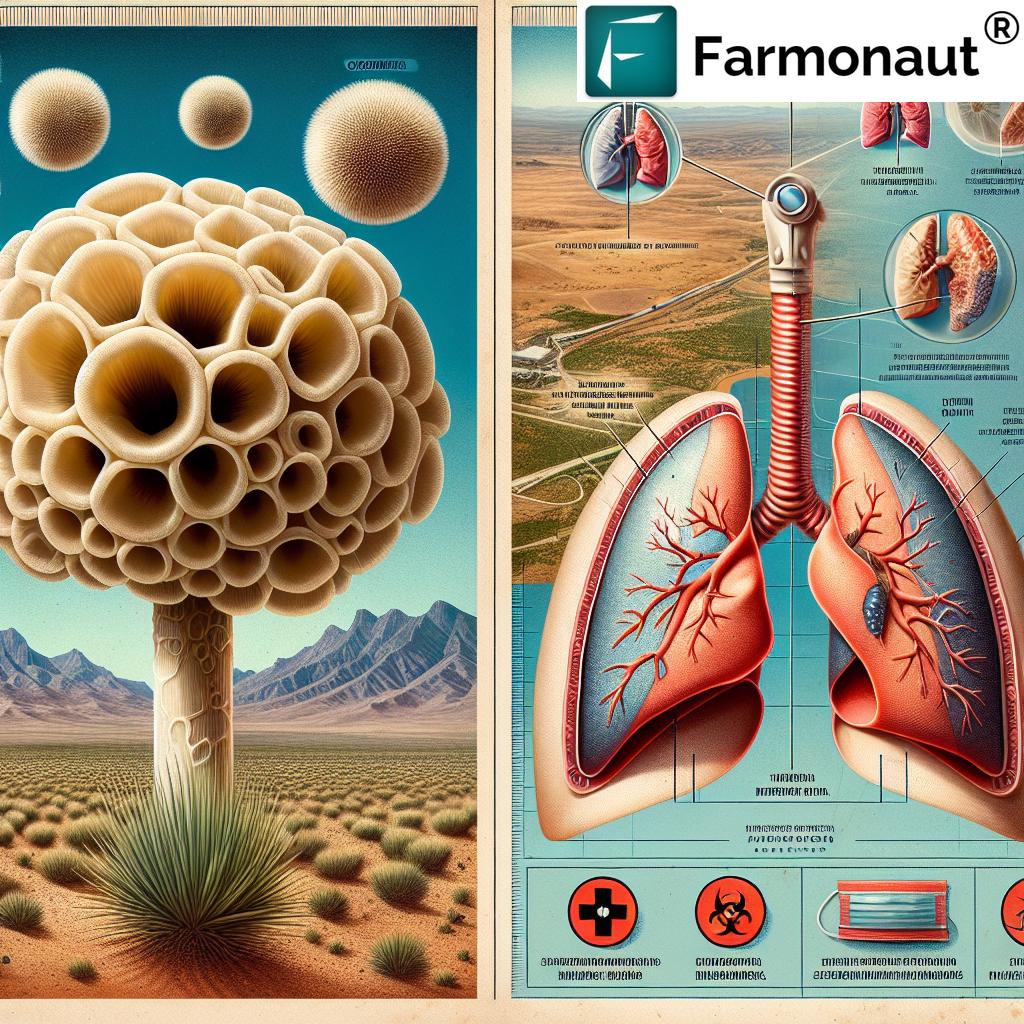
In the wake of the global COVID-19 pandemic, we are now facing a new health concern that demands our immediate attention. A groundbreaking medical study has revealed a concerning link between COVID-19 recovery and an increased risk of coccidioidomycosis, more commonly known as Valley Fever. This fungal infection, typically found in arid southwestern regions of the United States, is emerging as a potential threat to those who have recently battled COVID-19, especially individuals with compromised immune systems.
As we delve into this critical health issue, we’ll explore the symptoms, diagnosis, and treatment of Valley Fever in the context of post-COVID immune suppression. Our goal is to provide valuable insights for both medical practitioners and the public, shedding light on this emerging health concern and its implications for long-term COVID-19 management.
Understanding Valley Fever: A Silent Threat
Valley Fever, caused by the Coccidioides fungus, is a respiratory disease that begins when fungal spores are inhaled. These spores are commonly found in the soil of arid and semi-arid regions, particularly in the southwestern United States, parts of Mexico, and areas of Central and South America.
While many people who inhale these spores may remain asymptomatic or experience only mild symptoms, the disease can progress to severe respiratory illness in some cases. This is especially true for individuals with weakened immune systems, such as those recovering from COVID-19.
The COVID-19 Connection: A New Risk Factor
Recent findings from Baptist Hospitals of Southeast Texas have highlighted a disturbing trend: individuals recovering from COVID-19 may be at a heightened risk for coccidioidomycosis infections. This connection is particularly alarming given the widespread nature of the COVID-19 pandemic and the potential for long-term health implications.
The case study that brought this issue to light involved a 68-year-old man who developed disseminated coccidioidomycosis following a recent COVID-19 infection and travel to endemic regions. His experience underscores the need for greater awareness among both healthcare professionals and the general public.
Post-COVID-19 Immune Vulnerabilities
COVID-19 has been shown to disrupt the immune system in profound ways. The virus can suppress normal immune responses, creating a fertile ground for secondary infections. This is particularly relevant for fungal diseases like Valley Fever, which rely on an impaired immune system to spread and cause severe symptoms.
The overlap in symptoms between COVID-19 and fungal infections can delay accurate diagnosis. Common symptoms such as fever, cough, and fatigue are shared by both conditions, making it challenging for healthcare providers to differentiate between the two without specific testing.
Valley Fever Symptoms: A Closer Look
Understanding the symptoms of Valley Fever is crucial for early detection and treatment, especially in the context of post-COVID recovery. Here are some key symptoms to be aware of:
- Fever
- Cough
- Fatigue
- Shortness of breath
- Chest pain
- Headache
- Night sweats
- Joint aches and muscle pain
- Skin rash
It’s important to note that these symptoms can vary in severity and may mimic other respiratory conditions, including COVID-19 itself. This similarity in presentation underscores the importance of thorough diagnostic evaluations, especially for individuals with a history of COVID-19 and travel to endemic regions.
Diagnosis Challenges: Unraveling the Mystery
Diagnosing Valley Fever in post-COVID patients presents unique challenges. The case study highlighted earlier demonstrates the complexity of this issue. The patient initially received treatments for bacterial pneumonia, illustrating how easily Valley Fever can be mistaken for other respiratory conditions.
Key diagnostic tools for Valley Fever include:
- Blood tests to detect Coccidioides antibodies
- Chest X-rays or CT scans to identify lung abnormalities
- Sputum cultures to isolate the fungus
- In some cases, tissue biopsies may be necessary
Healthcare providers must maintain a high index of suspicion for Valley Fever, especially when evaluating patients with a history of COVID-19 and travel to endemic areas.
Treatment Approaches: Combating Valley Fever
Once diagnosed, Valley Fever requires prompt and appropriate treatment. The approach to treatment may vary depending on the severity of the infection and the patient’s overall health status. Common treatment strategies include:
- Antifungal medications such as fluconazole, itraconazole, or amphotericin B
- Supportive care to manage symptoms and prevent complications
- Close monitoring of liver function, as some antifungal medications can affect the liver
- In severe cases, hospitalization may be necessary
The case study patient responded well to a five-day course of amphotericin B, followed by long-term fluconazole therapy. This highlights the importance of tailored treatment plans based on individual patient needs and disease progression.
“COVID-19 recovery increases Valley Fever risk by an estimated 50% in endemic areas of the southwestern United States.”
The Role of Travel in Valley Fever Cases
Travel history plays a crucial role in the risk assessment and diagnosis of Valley Fever, especially in the context of post-COVID recovery. The case study patient’s recent visits to endemic regions like Arizona, Nevada, and Mexico significantly increased his risk of exposure to Coccidioides spores.
This underscores the importance of:
- Thorough travel history documentation during medical evaluations
- Awareness of Valley Fever endemic regions among healthcare providers
- Patient education about the risks associated with travel to these areas, especially for those with compromised immune systems
Travelers to endemic regions, particularly those recovering from COVID-19, should take precautions such as avoiding activities that disturb soil and dust, and wearing protective masks when necessary.
Broader Implications for Healthcare
The emerging link between COVID-19 recovery and increased susceptibility to Valley Fever has significant implications for healthcare practices and public health strategies.
Key considerations include:
- Enhanced screening protocols for post-COVID patients, especially those with travel history to endemic regions
- Increased awareness and education among healthcare providers about the potential for fungal infections in COVID-19 survivors
- Development of more rapid and accurate diagnostic tools for fungal infections
- Research into the long-term effects of COVID-19 on immune function and susceptibility to secondary infections
- Public health campaigns to educate at-risk populations about the potential dangers of fungal infections post-COVID
Comparative Symptom Chart: COVID-19 vs. Valley Fever
| Symptoms | COVID-19 | Valley Fever |
|---|---|---|
| Fever | ✓ | ✓ |
| Cough | ✓ | ✓ |
| Fatigue | ✓ | ✓ |
| Shortness of breath | ✓ | ✓ |
| Body aches | ✓ | ✓ |
| Loss of taste/smell | ✓ | ✗ |
| Skin rash | ✗ | ✓ |
| Night sweats | ✗ | ✓ |
This chart illustrates the significant overlap in symptoms between COVID-19 and Valley Fever, highlighting the diagnostic challenges faced by healthcare providers. The similarity in presentation underscores the need for thorough evaluation and testing, especially in patients with a history of COVID-19 and travel to endemic regions.
Prevention Strategies: Protecting Yourself and Others
While it may not be possible to completely eliminate the risk of Valley Fever, especially in endemic areas, there are steps that individuals can take to reduce their exposure and protect their health:
- Avoid activities that generate dust in areas where Valley Fever is common
- Wear a N95 respirator mask when in dusty environments
- Stay indoors during dust storms
- Keep windows and doors closed during windy conditions
- Use air filtration systems in homes and vehicles
- Maintain a healthy lifestyle to support immune function
- If recovering from COVID-19, be extra vigilant about potential fungal infection symptoms
For healthcare providers, prevention strategies include:
- Maintaining a high index of suspicion for Valley Fever in post-COVID patients from endemic areas
- Implementing comprehensive screening protocols
- Educating patients about the potential risks and symptoms to watch for
- Collaborating with infectious disease specialists when necessary
The Future of Research and Treatment
The discovery of the link between COVID-19 recovery and increased Valley Fever risk opens up new avenues for research and treatment development. Some key areas of focus include:
- Understanding the specific mechanisms by which COVID-19 increases susceptibility to fungal infections
- Developing more effective and targeted antifungal treatments
- Exploring the potential for preventive measures or treatments for high-risk individuals
- Investigating the long-term impacts of COVID-19 on immune function and overall health
- Improving diagnostic tools to differentiate between viral, bacterial, and fungal infections more quickly and accurately
As we continue to navigate the complex landscape of post-COVID health challenges, ongoing research and collaboration between healthcare providers, researchers, and public health officials will be crucial in addressing the emerging threat of Valley Fever and other secondary infections.
Conclusion: Vigilance and Awareness in the Post-COVID Era
The emergence of Valley Fever as a potential threat to COVID-19 survivors underscores the complex and evolving nature of the pandemic’s impact on public health. As we continue to learn more about the long-term effects of COVID-19, it’s clear that our approach to patient care and public health strategies must evolve as well.
Key takeaways from this exploration of Valley Fever risk in post-COVID patients include:
- The importance of maintaining a high index of suspicion for fungal infections in COVID-19 survivors, especially those with travel history to endemic regions
- The need for comprehensive diagnostic evaluations that consider both viral and fungal infections
- The critical role of patient education and awareness in early detection and treatment
- The ongoing need for research into the long-term impacts of COVID-19 on immune function and susceptibility to secondary infections
As we move forward, it’s crucial that healthcare providers, patients, and the general public remain vigilant and informed about the potential risks associated with Valley Fever and other opportunistic infections in the wake of COVID-19. By staying alert, promoting awareness, and continuing to advance our understanding of these complex health issues, we can work together to protect vulnerable populations and improve outcomes for all.
FAQ Section
Q: What is Valley Fever?
A: Valley Fever is a fungal infection caused by inhaling spores of the Coccidioides fungus, commonly found in the soil of arid regions in the southwestern United States, Mexico, and parts of Central and South America.
Q: How does COVID-19 increase the risk of Valley Fever?
A: COVID-19 can suppress the immune system, making individuals more susceptible to secondary infections like Valley Fever. This is especially true for those with compromised immune systems or those who have recently recovered from severe COVID-19.
Q: What are the common symptoms of Valley Fever?
A: Common symptoms include fever, cough, fatigue, shortness of breath, chest pain, headache, night sweats, joint aches, and skin rash. However, these can vary in severity and may mimic other respiratory conditions.
Q: How is Valley Fever diagnosed?
A: Diagnosis typically involves blood tests to detect Coccidioides antibodies, chest X-rays or CT scans, sputum cultures, and in some cases, tissue biopsies.
Q: What is the treatment for Valley Fever?
A: Treatment usually involves antifungal medications such as fluconazole, itraconazole, or amphotericin B, along with supportive care to manage symptoms and prevent complications.
Q: Can Valley Fever be prevented?
A: While it’s difficult to completely prevent exposure in endemic areas, risk can be reduced by avoiding activities that generate dust, wearing N95 respirator masks in dusty environments, and staying indoors during dust storms.
Q: Who is most at risk for Valley Fever?
A: Individuals living in or traveling to endemic areas are at risk, with increased risk for those with weakened immune systems, including recent COVID-19 survivors, older adults, and those with chronic health conditions.
Q: How long does Valley Fever treatment typically last?
A: Treatment duration can vary widely depending on the severity of the infection and the individual’s overall health. It can range from a few months to a year or more in severe cases.
Q: Can Valley Fever recur after treatment?
A: While recurrence is possible, especially in immunocompromised individuals, most people who receive appropriate treatment recover fully without recurrence.
Q: How can healthcare providers better identify Valley Fever in post-COVID patients?
A: Healthcare providers should maintain a high index of suspicion for Valley Fever, especially in patients with a history of COVID-19 and travel to endemic areas. Comprehensive screening protocols and thorough travel history documentation are crucial.
Earn With Farmonaut: Earn 20% recurring commission with Farmonaut’s affiliate program by sharing your promo code and helping farmers save 10%. Onboard 10 Elite farmers monthly to earn a minimum of $148,000 annually—start now and grow your income!
For more information on agricultural technology and innovative farming solutions, visit Farmonaut’s web app or download our mobile apps:
For developers interested in integrating agricultural data into their applications, check out our API and API Developer Docs.